Research impact and public engagement
Driven by the expertise of Teesside University's community of academics, our research aims to have a positive impact on the economic, social and cultural success of students, partners and the communities we serve.
From shaping global public health policies on obesity, physical activity and jet lag, to increasing cultural engagement, transforming the digital capabilities of the construction sector and tackling organised crime, our research addresses some of the most complex issues facing the world around us.
But we don't do any of this alone. Our researchers partner and collaborate with businesses, charities, local and national governments and members of the public, ensuring that all our work has relevance and value beyond the university - whether that's locally, nationally or on a global scale.
Our approach to research impact is underpinned be the Teesside University Impact Framework that outlines the values and behaviours, capabilities and competencies, and mechanisms for advancing research impact, ensuring we maximise the potential of our research and the benefits of research to our communities and stakeholders.
Evaluation and Impact Team
Formed in April 2019 to meet the demand by external agencies for research that informs and benefits the local and regional economy
Impact Acceleration Account
Teesside University has been awarded an AHRC Impact Acceleration Account (IAA).
Public and Community Engagement
Public Engagement is central to all our activities whether research, enterprise, and knowledge exchange, leaning and teaching or wider university operation as an anchor institution with a civic mission.
Impact case studies
The case studies below demonstrate the far-reaching impact of our research.
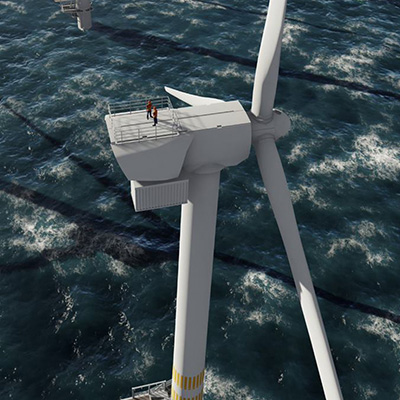
A smarter approach for the energy sector
Harnessing Industry 4.0 to better integrate renewable energy plants across power networks...
More

Creating 'useful museums'
Reimagining the role of communities in curating museums and galleries...
More

Improving access to justice for vulnerable people
Exploring the role of rapport-building and intermediaries in engaging vulnerable individuals in the ...
More

Managing data in the built environment
Using novel digital technologies to manage information flow in complex construction and engineering ...
More

Promoting gender equality in writing and research
An immersive three-day workshop focused on advancing the research careers of next generation women ...
More

Taking the construction industry to new heights
Using novel digital tools to embed building information modelling (BIM) capabilities in the ...
More
If you are interested in finding out more about any of our research impact please contact us.
ref@tees.ac.uk








